beta-Artemether
- 71963-77-4
- Artemether (SM-224)
- Artesaph
- Falcidol
- Gvither
- Create:2005-08-01
- Modify:2025-01-18
 Artemether (annotation moved to).
Artemether (annotation moved to).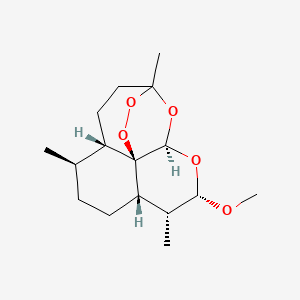
- alpha Artemether
- alpha-Artemether
- artemether
- artemether, (3R-(3alpha,5abeta,6alpha,8abeta,9alpha,10beta,12beta,12aR*))-isomer
- artemether, (3R-(3alpha,5abeta,6beta,8aalpha,9alpha,10beta,12beta,12aR*))-isomer
- artemether, (3R-(3alpha,5abeta,6beta,8abeta,9alpha,10alpha,12beta,12aR*))-isomer
- artenam
- beta Arthemeter
- beta-arthemeter
- O Methyldihydroartemisinine
- O-methyldihydroartemisinine
- 71963-77-4
- Artemether (SM-224)
- Artesaph
- Falcidol
- Gvither
- Larither
- Malartem
- .beta.-Artemether
- Artemether [INN]
- C7D6T3H22J
- SM224
- ss-Artemether
- NSC-665970
- NSC-759820
- ARTEMETHER [MI]
- ARTEMETHER [JAN]
- ARTEMETHER [HSDB]
- ARTEMETHER [USAN]
- (+)-ARTEMETHER
- ARTEMETHER [VANDF]
- ARTEMETHER [MART.]
- ARTEMETHER [USP-RS]
- ARTEMETHER [WHO-DD]
- ARTEMETHER [WHO-IP]
- Dihydroqinghaosu methyl ether;Dihydroartemisinin methyl ether;SM224
- ARTEMETHER [ORANGE BOOK]
- SCHEMBL19967613
- COARTEM COMPONENT ARTEMETHER
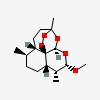
- (3R,5aS,6R,8aS,9R,10S,12R,12aR)-Decahydro-10-methoxy-3,6,9-trimethyl-3,12-epoxy-12H-pyrano(4,3-j)-1,2-benzodioxepin
- 3,12-Epoxy-12H-pyrano(4,3-j)-1,2-benzodioxepin, decahydro-10-methoxy-3,6,9-trimethyl-, (3R,5aS,6R,8aS,9R,10S,12R,12aR)-
- ARTEMETHERUM [WHO-IP LATIN]
- MFCD00866205
- .beta.-Dihydroartemisinin methyl ether
- AKOS016339568
- KS-5314
- AS-11606
- A2190
- (3R,5aS,6R,8aS,9R,10S,12R,12aR)-10-Methoxy-3,6,9-trimethyldecahydro-3,12-epoxypyrano[4,3-j]-1,2-benzodioxepine
 Artemether (annotation moved to)
Artemether (annotation moved to)
P264, P270, P301+P317, P330, and P501
(The corresponding statement to each P-code can be found at the GHS Classification page.)
Aggregated GHS information provided per 41 reports by companies from 3 notifications to the ECHA C&L Inventory.
Reported as not meeting GHS hazard criteria per 1 of 41 reports by companies. For more detailed information, please visit ECHA C&L website.
There are 2 notifications provided by 40 of 41 reports by companies with hazard statement code(s).
Information may vary between notifications depending on impurities, additives, and other factors. The percentage value in parenthesis indicates the notified classification ratio from companies that provide hazard codes. Only hazard codes with percentage values above 10% are shown.
Patents are available for this chemical structure:
https://patentscope.wipo.int/search/en/result.jsf?inchikey=SXYIRMFQILZOAM-GXTLMGRASA-N
- Drug Gene Interaction database (DGIdb)LICENSEThe data used in DGIdb is all open access and where possible made available as raw data dumps in the downloads section.http://www.dgidb.org/downloadsARTEMETHERhttps://www.dgidb.org/drugs/rxcui:18343
- European Chemicals Agency (ECHA)LICENSEUse of the information, documents and data from the ECHA website is subject to the terms and conditions of this Legal Notice, and subject to other binding limitations provided for under applicable law, the information, documents and data made available on the ECHA website may be reproduced, distributed and/or used, totally or in part, for non-commercial purposes provided that ECHA is acknowledged as the source: "Source: European Chemicals Agency, http://echa.europa.eu/". Such acknowledgement must be included in each copy of the material. ECHA permits and encourages organisations and individuals to create links to the ECHA website under the following cumulative conditions: Links can only be made to webpages that provide a link to the Legal Notice page.https://echa.europa.eu/web/guest/legal-noticeARTEMETHER (EC: 663-549-0)https://echa.europa.eu/information-on-chemicals/cl-inventory-database/-/discli/details/194770
- FDA Global Substance Registration System (GSRS)LICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linking
- Hazardous Substances Data Bank (HSDB)
- FDA Pharm ClassesLICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linkingFDA Pharmacological Classificationhttps://www.fda.gov/ForIndustry/DataStandards/StructuredProductLabeling/ucm162549.htm
- Natural Product Activity and Species Source (NPASS)
- NCI Thesaurus (NCIt)LICENSEUnless otherwise indicated, all text within NCI products is free of copyright and may be reused without our permission. Credit the National Cancer Institute as the source.https://www.cancer.gov/policies/copyright-reuseNCI Thesaurushttps://ncit.nci.nih.gov
- NLM RxNorm TerminologyLICENSEThe RxNorm Terminology is created by the National Library of Medicine (NLM) and is in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from NLM. Credit to the U.S. National Library of Medicine as the source is appreciated but not required. The full RxNorm dataset requires a free license.https://www.nlm.nih.gov/research/umls/rxnorm/docs/termsofservice.html
- Medical Subject Headings (MeSH)LICENSEWorks produced by the U.S. government are not subject to copyright protection in the United States. Any such works found on National Library of Medicine (NLM) Web sites may be freely used or reproduced without permission in the U.S.https://www.nlm.nih.gov/copyright.htmlAntimalarialshttps://www.ncbi.nlm.nih.gov/mesh/68000962
- PubChem
- GHS Classification (UNECE)GHS Classification Treehttp://www.unece.org/trans/danger/publi/ghs/ghs_welcome_e.html
- PATENTSCOPE (WIPO)SID 397256568https://pubchem.ncbi.nlm.nih.gov/substance/397256568
- NCBI