Canagliflozin
- Canagliflozin
- 842133-18-0
- Invokana
- Canagliflozin anhydrous
- TA-7284
- Create:2008-06-23
- Modify:2025-01-18
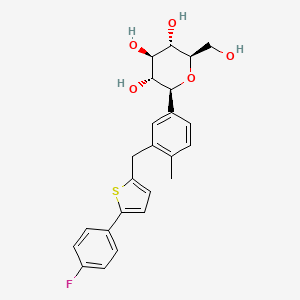
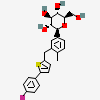
- 1-(Glucopyranosyl)-4-methyl-3-(5-(4-fluorophenyl)-2-thienylmethyl)benzene - T777973
- canagliflozin
- Canagliflozin Hemihydrate
- Canagliflozin, Anhydrous
- Invokana
- Canagliflozin
- 842133-18-0
- Invokana
- Canagliflozin anhydrous
- TA-7284
- JNJ-28431754
- Canagliflozin [INN]
- (2S,3R,4R,5S,6R)-2-(3-((5-(4-FLUOROPHENYL)THIOPHEN-2-YL)METHYL)-4-METHYLPHENYL)-6-(HYDROXYMETHYL)TETRAHYDRO-2H-PYRAN-3,4,5-TRIOL
- Canagliflozin hydrate
- 1-(Glucopyranosyl)-4-methyl-3-(5-(4-fluorophenyl)-2-thienylmethyl)benzene
- D-Glucitol,1,5-anhydro-1-C-[3-[[5-(4-fluorophenyl)-2-thienyl]methyl]-4-methylphenyl]-, (1S)-
- CHEBI:73274
- 6S49DGR869
- (2S,3R,4R,5S,6R)-2-[3-[[5-(4-fluorophenyl)thiophen-2-yl]methyl]-4-methylphenyl]-6-(hydroxymethyl)oxane-3,4,5-triol
- TA 7284
- (1S)-1,5-Anhydro-1-(3-((5-(4-fluorophenyl)-2-thienyl)methyl)-4-methylphenyl)-D-glucitol
- (1S)-1,5-anhydro-1-(3-{[5-(4-fluorophenyl)-2-thienyl]methyl}-4-methylphenyl)-D-glucitol
- (1S)-1,5-Anhydro-1-C-[3-[[5-(4-fluorophenyl)-2-thienyl]methyl]-4-methylphenyl]-D-glucitol
- JNJ 28431754
- MFCD18251436
- (1s)-1,5-anhydro-1-c-(3-((5-(4-fluorophenyl)-2-thienyl)methyl)-4-methylphenyl)-d-glucitol
- (2S,3R,4R,5S,6R)-2-(3-{[5-(4-fluorophenyl)thiophen-2-yl]methyl}-4-methylphenyl)-6-(hydroxymethyl)oxane-3,4,5-triol
- JNJ 24831754ZAE
- UNII-6S49DGR869
- JNJ 24831754AAA
- JNJ 24831754
- Canagliflozin (Standard)
- CANAGLIFLOZIN [MI]
- MLS006011126
- SCHEMBL157162
- CANAGLIFLOZIN [WHO-DD]
- GTPL4582
- CHEMBL2048484
- HSDB 8284
- BCPP000303
- DTXSID601004469
- BDBM50386885
- HY-10451R
- s2760
- AKOS025401827
- BCP9000477
- CCG-229581
- CS-0522
- DB08907
- KS-1443
- NCGC00346691-02
- (1S)-1,5-Anhydro-1-c-(3-((5-(4-fluorophenyl)thiophen-2-yl)methyl)-4-methylphenyl)-D-glucitol
- AC-26303
- HY-10451
- SMR004702906
- NS00099376
- SW219119-1
- EN300-6733492
- J-500391
- Q5030940
- BRD-K90868879-001-02-0
- BRD-K90868879-001-03-8
- Z2235801995
- (1S)-1,5-anhydro-1-(3-{[5-(4-fluorophenyl)-2-thienyl]methyl}-4-methyl-phenyl)-D-glucitol
- (1S)-1,5-ANHYDRO-1-C-(3-((5-(4-FLUOROPHENYL)THIOPHEN-2-YL)METHYL)-4-METHYLPHENYL)-D- GLUCITOL
- D-Glucitol, 1,5-anhydro-1-C-(3-((5-(4-fluorophenyl)-2-thienyl)methyl)-4- methylphenyl)-, (1S)-
- D-glucitol, 1,5-anhydro-1-c-(3-((5-(4-fluorophenyl)-2-thienyl)methyl)-4- methylphenyl)-, (1s)-
- D-GLUCITOL, 1,5-ANHYDRO-1-C-(3-((5-(4-FLUOROPHENYL)-2-THIENYL)METHYL)-4-METHYLPHENYL)-
- JNJ 24831754ZAE , JNJ 28431754AAA , TA 7284 , JNJ 28431754




H302 (60%): Harmful if swallowed [Warning Acute toxicity, oral]
H318 (20%): Causes serious eye damage [Danger Serious eye damage/eye irritation]
H319 (60%): Causes serious eye irritation [Warning Serious eye damage/eye irritation]
H361 (80%): Suspected of damaging fertility or the unborn child [Warning Reproductive toxicity]
H362 (20%): May cause harm to breast-fed children [Reproductive toxicity, effects on or via lactation]
H411 (80%): Toxic to aquatic life with long lasting effects [Hazardous to the aquatic environment, long-term hazard]
P203, P260, P263, P264, P264+P265, P270, P273, P280, P301+P317, P305+P351+P338, P305+P354+P338, P317, P318, P330, P337+P317, P391, P405, and P501
(The corresponding statement to each P-code can be found at the GHS Classification page.)
Aggregated GHS information provided per 5 reports by companies from 4 notifications to the ECHA C&L Inventory. Each notification may be associated with multiple companies.
Information may vary between notifications depending on impurities, additives, and other factors. The percentage value in parenthesis indicates the notified classification ratio from companies that provide hazard codes. Only hazard codes with percentage values above 10% are shown.
Acute Tox. 4 (60%)
Eye Dam. 1 (20%)
Eye Irrit. 2 (60%)
Repr. 2 (80%)
Lact. (20%)
Aquatic Chronic 2 (80%)
◉ Summary of Use during Lactation
No information is available on the clinical use of canagliflozin during breastfeeding. Canagliflozin is 99% protein bound in plasma, so it is unlikely to pass into breastmilk in clinically important amounts. The manufacturer does not recommend canagliflozin during breastfeeding because of a theoretical risk to the infant's developing kidney. An alternate drug may be preferred, especially while nursing a newborn or preterm infant.
◉ Effects in Breastfed Infants
Relevant published information was not found as of the revision date.
◉ Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Patents are available for this chemical structure:
https://patentscope.wipo.int/search/en/result.jsf?inchikey=XTNGUQKDFGDXSJ-ZXGKGEBGSA-N
- Avoid alcohol. Excess alcohol intake may promote ketoacidosis.
- Drink plenty of fluids.
- Take before a meal. It is recommended to take this drug before the first meal of the day.
- CAS Common ChemistryLICENSEThe data from CAS Common Chemistry is provided under a CC-BY-NC 4.0 license, unless otherwise stated.https://creativecommons.org/licenses/by-nc/4.0/
- ChemIDplusChemIDplus Chemical Information Classificationhttps://pubchem.ncbi.nlm.nih.gov/source/ChemIDplus
- DrugBankLICENSECreative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode)https://www.drugbank.ca/legal/terms_of_useCanagliflozinhttps://www.drugbank.ca/drugs/DB08907
- EPA DSSToxCanagliflozinhttps://comptox.epa.gov/dashboard/DTXSID601004469CompTox Chemicals Dashboard Chemical Listshttps://comptox.epa.gov/dashboard/chemical-lists/
- European Chemicals Agency (ECHA)LICENSEUse of the information, documents and data from the ECHA website is subject to the terms and conditions of this Legal Notice, and subject to other binding limitations provided for under applicable law, the information, documents and data made available on the ECHA website may be reproduced, distributed and/or used, totally or in part, for non-commercial purposes provided that ECHA is acknowledged as the source: "Source: European Chemicals Agency, http://echa.europa.eu/". Such acknowledgement must be included in each copy of the material. ECHA permits and encourages organisations and individuals to create links to the ECHA website under the following cumulative conditions: Links can only be made to webpages that provide a link to the Legal Notice page.https://echa.europa.eu/web/guest/legal-notice(2S,3R,4R,5S,6R)-2-(3-{[5-(4-fluorophenyl)thiophen-2-yl]methyl}-4-methylphenyl)-6-(hydroxymethyl)oxane-3,4,5-triolhttps://echa.europa.eu/substance-information/-/substanceinfo/100.223.671(2S,3R,4R,5S,6R)-2-(3-{[5-(4-fluorophenyl)thiophen-2-yl]methyl}-4-methylphenyl)-6-(hydroxymethyl)oxane-3,4,5-triol (EC: 695-192-1)https://echa.europa.eu/information-on-chemicals/cl-inventory-database/-/discli/details/229660
- FDA Global Substance Registration System (GSRS)LICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linkingCANAGLIFLOZIN ANHYDROUShttps://gsrs.ncats.nih.gov/ginas/app/beta/substances/6S49DGR869
- Hazardous Substances Data Bank (HSDB)Canagliflozinhttps://pubchem.ncbi.nlm.nih.gov/source/hsdb/8284
- ChEBI
- FDA Pharm ClassesLICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linkingCANAGLIFLOZIN ANHYDROUShttps://dailymed.nlm.nih.gov/dailymed/browse-drug-classes.cfmFDA Pharmacological Classificationhttps://www.fda.gov/ForIndustry/DataStandards/StructuredProductLabeling/ucm162549.htm
- NCI Thesaurus (NCIt)LICENSEUnless otherwise indicated, all text within NCI products is free of copyright and may be reused without our permission. Credit the National Cancer Institute as the source.https://www.cancer.gov/policies/copyright-reuseNCI Thesaurushttps://ncit.nci.nih.gov
- Open TargetsLICENSEDatasets generated by the Open Targets Platform are freely available for download.https://platform-docs.opentargets.org/licenceCANAGLIFLOZIN ANHYDROUShttps://platform.opentargets.org/drug/CHEMBL2048484
- ChEMBLLICENSEAccess to the web interface of ChEMBL is made under the EBI's Terms of Use (http://www.ebi.ac.uk/Information/termsofuse.html). The ChEMBL data is made available on a Creative Commons Attribution-Share Alike 3.0 Unported License (http://creativecommons.org/licenses/by-sa/3.0/).http://www.ebi.ac.uk/Information/termsofuse.htmlChEMBL Protein Target Treehttps://www.ebi.ac.uk/chembl/g/#browse/targets
- ClinicalTrials.govLICENSEThe ClinicalTrials.gov data carry an international copyright outside the United States and its Territories or Possessions. Some ClinicalTrials.gov data may be subject to the copyright of third parties; you should consult these entities for any additional terms of use.https://clinicaltrials.gov/ct2/about-site/terms-conditions#Use
- Comparative Toxicogenomics Database (CTD)LICENSEIt is to be used only for research and educational purposes. Any reproduction or use for commercial purpose is prohibited without the prior express written permission of NC State University.http://ctdbase.org/about/legal.jsp
- IUPHAR/BPS Guide to PHARMACOLOGYLICENSEThe Guide to PHARMACOLOGY database is licensed under the Open Data Commons Open Database License (ODbL) https://opendatacommons.org/licenses/odbl/. Its contents are licensed under a Creative Commons Attribution-ShareAlike 4.0 International License (http://creativecommons.org/licenses/by-sa/4.0/)https://www.guidetopharmacology.org/about.jsp#licenseGuide to Pharmacology Target Classificationhttps://www.guidetopharmacology.org/targets.jsp
- Therapeutic Target Database (TTD)Canagliflozinhttps://idrblab.net/ttd/data/drug/details/D08DFX
- Crystallography Open Database (COD)LICENSEAll data in the COD and the database itself are dedicated to the public domain and licensed under the CC0 License. Users of the data should acknowledge the original authors of the structural data.https://creativecommons.org/publicdomain/zero/1.0/
- DailyMed
- European Medicines Agency (EMA)LICENSEInformation on the European Medicines Agency's (EMA) website is subject to a disclaimer and copyright and limited reproduction notices.https://www.ema.europa.eu/en/about-us/legal-noticeInvokana (EMEA/H/C/002649)https://www.ema.europa.eu/en/medicines/human/EPAR/invokanacanagliflozin (P/0208/2022)https://www.ema.europa.eu/en/medicines/human/paediatric-investigation-plans/emea-001030-pip01-10-m10
- Drugs and Lactation Database (LactMed)Canagliflozinhttps://www.ncbi.nlm.nih.gov/books/n/lactmed/LM1060/
- Drugs@FDALICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linkingCANAGLIFLOZINhttps://www.accessdata.fda.gov/scripts/cder/daf/
- WHO Model Lists of Essential MedicinesLICENSEPermission from WHO is not required for the use of WHO materials issued under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Intergovernmental Organization (CC BY-NC-SA 3.0 IGO) license.https://www.who.int/about/policies/publishing/copyrightCanagliflozinhttps://list.essentialmeds.org/medicines/612
- EU Clinical Trials Register
- FDA Orange BookLICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linking
- WHO Anatomical Therapeutic Chemical (ATC) ClassificationLICENSEUse of all or parts of the material requires reference to the WHO Collaborating Centre for Drug Statistics Methodology. Copying and distribution for commercial purposes is not allowed. Changing or manipulating the material is not allowed.https://www.whocc.no/copyright_disclaimer/Canagliflozinhttps://www.whocc.no/atc_ddd_index/?code=A10BK02
- FDA Medication GuidesLICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linkingINVOKAMEThttps://dps.fda.gov/medguide
- National Drug Code (NDC) DirectoryLICENSEUnless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required.https://www.fda.gov/about-fda/about-website/website-policies#linking
- Japan Chemical Substance Dictionary (Nikkaji)
- Metabolomics Workbench
- NIPH Clinical Trials Search of Japan
- NLM RxNorm TerminologyLICENSEThe RxNorm Terminology is created by the National Library of Medicine (NLM) and is in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from NLM. Credit to the U.S. National Library of Medicine as the source is appreciated but not required. The full RxNorm dataset requires a free license.https://www.nlm.nih.gov/research/umls/rxnorm/docs/termsofservice.htmlcanagliflozinhttps://rxnav.nlm.nih.gov/id/rxnorm/1373458canagliflozin anhydroushttps://rxnav.nlm.nih.gov/id/rxnorm/1546031
- NORMAN Suspect List ExchangeLICENSEData: CC-BY 4.0; Code (hosted by ECI, LCSB): Artistic-2.0https://creativecommons.org/licenses/by/4.0/CANAGLIFLOZINNORMAN Suspect List Exchange Classificationhttps://www.norman-network.com/nds/SLE/
- PharosLICENSEData accessed from Pharos and TCRD is publicly available from the primary sources listed above. Please respect their individual licenses regarding proper use and redistribution.https://pharos.nih.gov/aboutcanagliflozinhttps://pharos.nih.gov/ligands/T8JXNHG58WMVCanagliflozinhttps://pharos.nih.gov/ligands/VFU1M6H1Z3A7
- Protein Data Bank in Europe (PDBe)
- RCSB Protein Data Bank (RCSB PDB)LICENSEData files contained in the PDB archive (ftp://ftp.wwpdb.org) are free of all copyright restrictions and made fully and freely available for both non-commercial and commercial use. Users of the data should attribute the original authors of that structural data.https://www.rcsb.org/pages/policies
- Springer Nature
- Thieme ChemistryLICENSEThe Thieme Chemistry contribution within PubChem is provided under a CC-BY-NC-ND 4.0 license, unless otherwise stated.https://creativecommons.org/licenses/by-nc-nd/4.0/
- Wikidatacanagliflozinhttps://www.wikidata.org/wiki/Q5030940
- WikipediaCanagliflozinhttps://en.wikipedia.org/wiki/Canagliflozin
- Medical Subject Headings (MeSH)LICENSEWorks produced by the U.S. government are not subject to copyright protection in the United States. Any such works found on National Library of Medicine (NLM) Web sites may be freely used or reproduced without permission in the U.S.https://www.nlm.nih.gov/copyright.htmlCanagliflozinhttps://www.ncbi.nlm.nih.gov/mesh/2009899Sodium-Glucose Transporter 2 Inhibitorshttps://www.ncbi.nlm.nih.gov/mesh/2027927
- PubChemPFAS and Fluorinated Compounds in PubChemhttps://gitlab.com/uniluxembourg/lcsb/eci/pubchem-docs/-/raw/main/pfas-tree/PFAS_Tree.pdf?inline=false
- GHS Classification (UNECE)GHS Classification Treehttp://www.unece.org/trans/danger/publi/ghs/ghs_welcome_e.html
- MolGenieMolGenie Organic Chemistry Ontologyhttps://github.com/MolGenie/ontology/
- PATENTSCOPE (WIPO)SID 403280719https://pubchem.ncbi.nlm.nih.gov/substance/403280719
- NCBI